NEWYou now have the option to listen to articles from reputable sources!
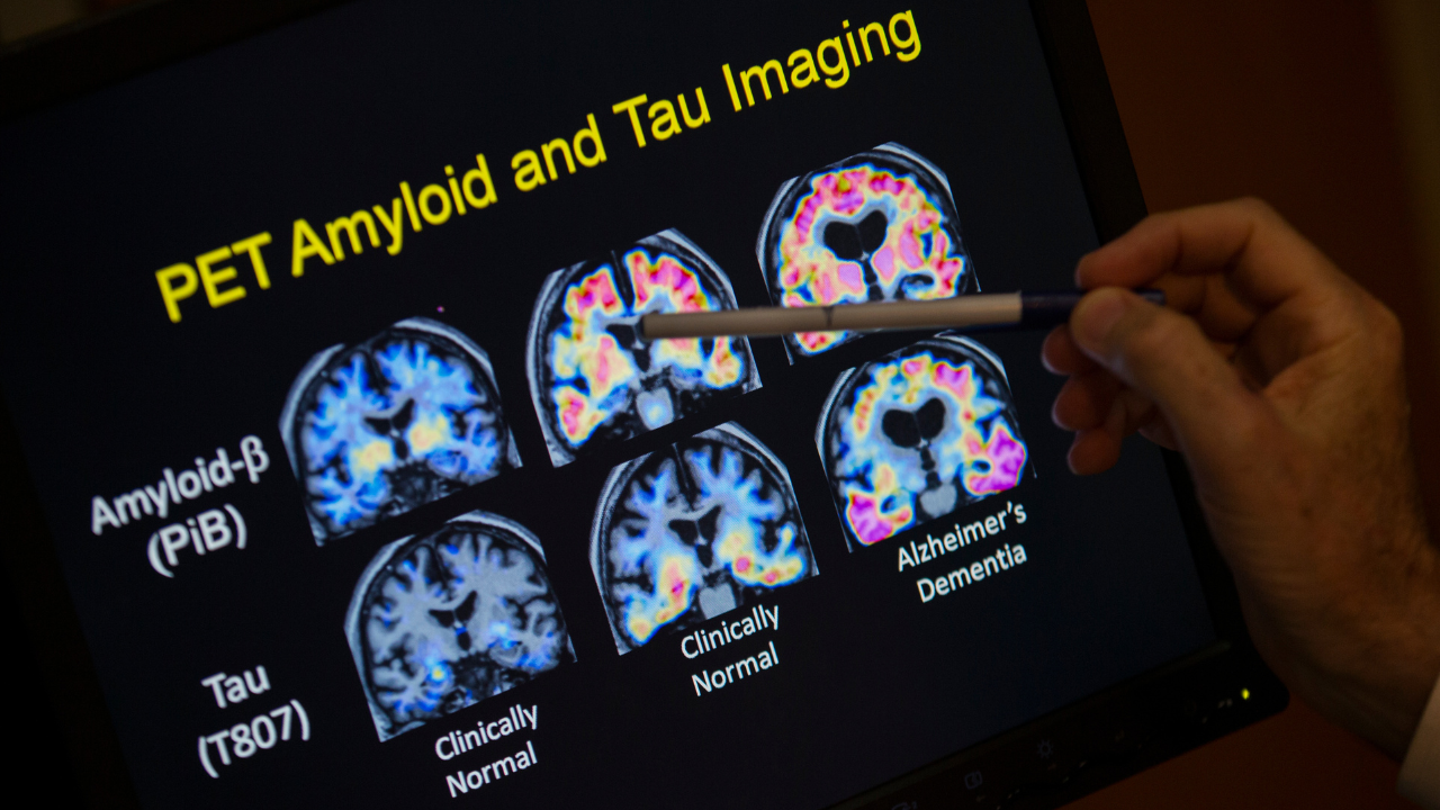
New research suggests that the brain possesses a hidden “sugar code” that could potentially lead to more effective treatments for neurological conditions such as Alzheimer’s disease.
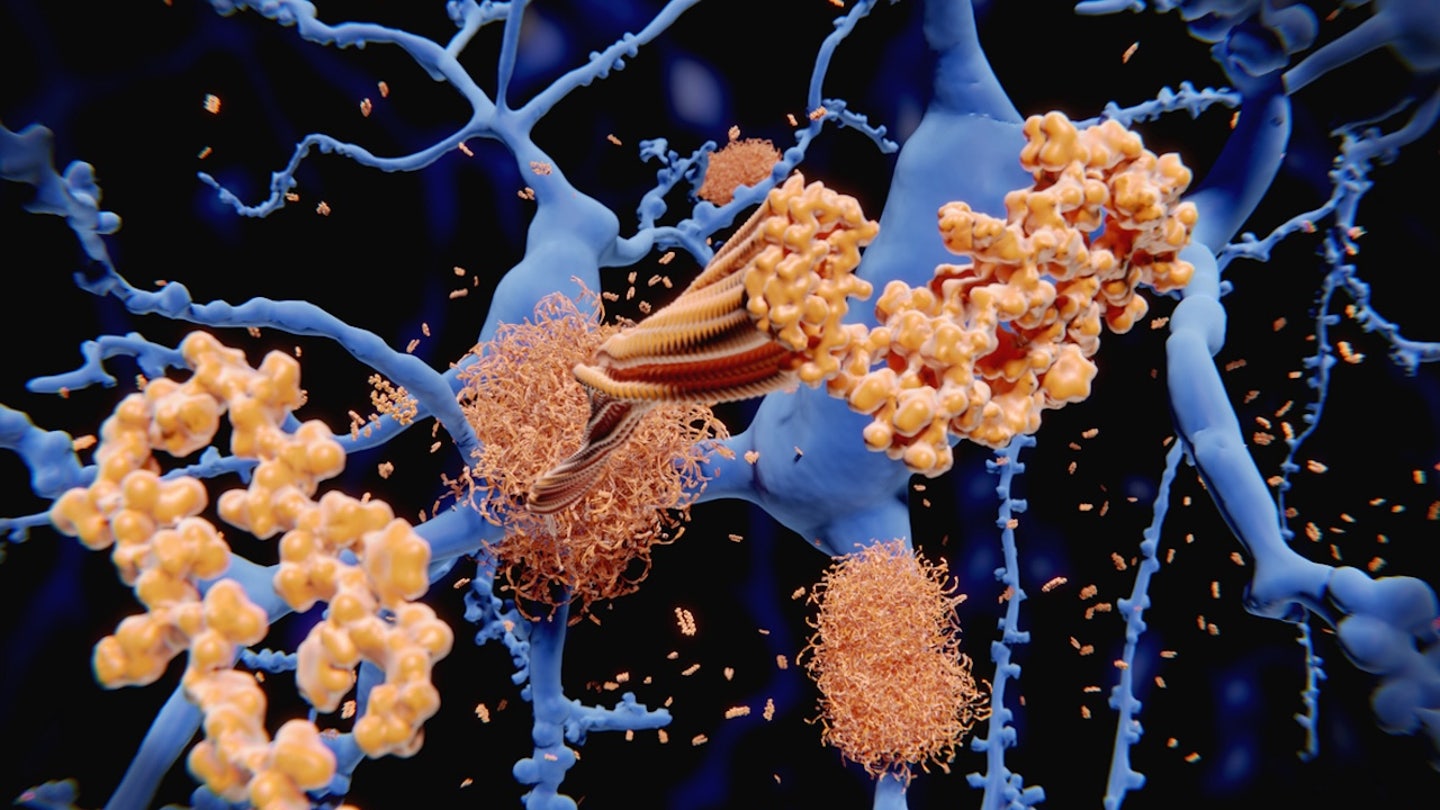
A recent study published in the journal Nature Metabolism has revealed that breaking down glycogen (stored glucose) in the brain may help reduce the accumulation of toxic proteins associated with common forms of dementia.
This groundbreaking study, led by Dr. Pankaj Kapahi, a professor at the Buck Institute for Research on Aging in California, sheds light on how glycogen could play a crucial role in influencing brain health and disease.
“The study began with fruit flies (Drosophila) that were genetically altered to mimic tauopathy, a condition characterized by the buildup of a protein called tau in the brain, similar to what occurs in Alzheimer’s disease,” explained Kapahi.
The study revealed that these modified flies exhibited brain damage and shortened lifespans, highlighting the detrimental effects of tau buildup.
New research suggests that breaking down glycogen in the brain could help reduce the accumulation of toxic proteins linked to Alzheimer’s disease. (iStock)
To validate the findings in human contexts, the research team also examined nerve cells derived from human patient cells with tau mutations, as well as postmortem brain samples from individuals with Alzheimer’s or related conditions.
Key Findings of the Study
In both the fly models and human models, researchers observed elevated levels of glycogen in the brain, along with indications of impaired glycogen breakdown, according to Kapahi.
This discovery was unexpected, as previous assumptions suggested that glycogen was primarily stored in muscles and the liver.
Furthermore, the study revealed that the excess glycogen contributed to disease progression. The tau proteins in the models interacted with glycogen, hindering its breakdown and impairing the nerves’ ability to combat cell damage.
However, by boosting an enzyme called glycogen phosphorylase (GlyP), which breaks down glycogen, researchers were able to mitigate damage to the fruit flies and human nerves.
“The next step in the process may involve neutralizing potentially harmful free radicals in our brains.”
The nerve cells utilized glycogen to protect against cell damage, suggesting that targeting enzymes responsible for sugar breakdown could hold promise for future therapeutic interventions.
The researchers also explored whether a restricted diet could promote better brain health in the flies.
Reducing the protein content in the insects’ diet resulted in increased longevity and improved brain health, indicating a link to enhanced glycogen breakdown.
The study found that breaking down glycogen in the brain could help reduce the accumulation of toxic proteins associated with Alzheimer’s disease. (AP Photo/Evan Vucci, File)
“We discovered that this improvement was linked to increased glycogen breakdown,” Kapahi stated.
Consequently, the primary finding of the study was that breaking down glycogen in neurons could shield the brain from damage caused by tau accumulation.
The scientists also developed a drug utilizing a special molecule called 8-Br-cAMP that mimicked the effects of dietary restriction, as highlighted in a press release.
The authors emphasized that while they are not currently advocating for low-protein diets, this research could lay the foundation for dietary or drug-based strategies to help slow the progression of Alzheimer’s and related disorders.

The study found that breaking down glycogen in neurons could protect the brain from damage caused by tau accumulation. (iStock)
Dr. Michael Okun, a neurologist from Florida and medical advisor to the Parkinson’s Foundation, commended the significance of the study’s findings.
“Rather than channeling sugar into energy-consuming processes, the breakdown of glycogen appeared to be redirected into a pathway that produces antioxidants,” noted Okun, author of “The Parkinson’s Plan,” in his comments to Fox News Digital.
“The subsequent step in this process could involve eliminating potentially harmful free radicals in our brains,” he added.

Alzheimer’s disease, the most prevalent form of dementia in the U.S., impacts over seven million individuals in the country. (iStock)
Okun confirmed that dietary restrictions activated a protective brain pathway and enhanced the breakdown of brain sugar.
“Ultimately, this led to a reduction in damage caused by the Alzheimer’s-related tau protein,” he remarked.
Study Constraints
The study, backed by the National Institutes of Health, the American Federation of Aging Research, and other sources, did have certain limitations, as acknowledged by the experts.
The researchers did not clarify whether breaking down brain glycogen could prevent human brain cells from undergoing cell death, according to Okun.
“It remains uncertain whether targeting glycogen breakdown will yield positive outcomes in human patients — and more importantly, whether it will be a safe approach.”
“We are still uncertain about why glycogen accumulates in diseases, or whether it serves as a cause or consequence of tau pathology — although our data hints at its potential role in amplifying disease progression,” Kapahi added.
Furthermore, the research was limited to fly and human cell models and has not yet been tested on living humans.
“We are still uncertain about why glycogen accumulates in diseases, or whether it serves as a cause or consequence of tau pathology — although our data hints at its potential role in amplifying disease progression,” the researcher explained. (iStock)
“It remains uncertain whether targeting glycogen breakdown will yield positive outcomes in human patients — and more importantly, whether it will be a safe approach,” Okun emphasized.
Alzheimer’s disease, the predominant form of dementia in the United States, affects more than seven million people in the country, as reported by the Alzheimer’s Association.
For more Health articles, visit www.foxnews.com/health
This neurological disorder impacts memory, cognition, and behavior. While there is currently no cure for the disease, certain medications can temporarily slow its progression and enhance quality of life.